Shoulder Instability
Mr. Richard Dallalana
MBBS FRACS FAOrthA
What is shoulder instability?
Shoulder instability refers to troublesome looseness of the shoulder joint. This may take the form of a single or multiple full dislocations, or episodes of partial dislocation (called subluxation). The unstable shoulder may result in pain without any actual dislocation having occurred. Over many years instability can lead to arthritis of the shoulder joint.
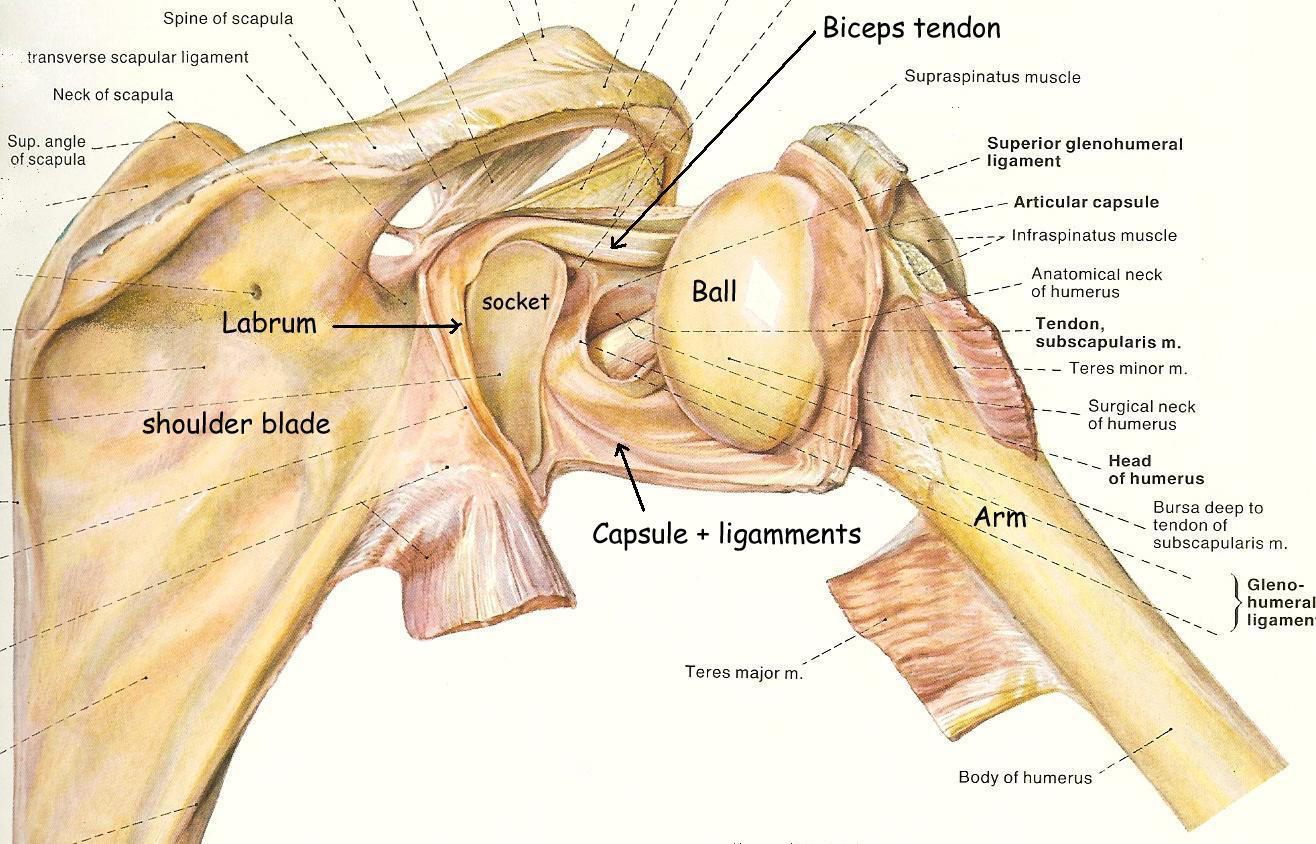
Anatomy of the shoulder (see fig. 1)
The main part of the shoulder consists of the ball at the top of the arm (humerus) which sits in a shallow socket (glenoid) connected to the shoulder blade (scapula). The socket has a ring of cartilage (labrum) around its edge which deepens it and helps keep the ball in it.
Surrounding the shoulder joint is a watertight sac called the joint capsule. The joint capsule holds in fluids that lubricate the joint. The walls of this capsule are made up of ligaments. These ligaments loosely connect the ball to the socket and attach to the ring of cartilage (labrum) at its edge. They become tight if the shoulder rotates too far in any direction and prevent the ball slipping out of the socket (a dislocation).
One of the biceps tendons enters the shoulder and attaches to the ring of cartilage near the top of the socket.
Fig.1 Shoulder joint opened from behind
Structural Damage to the shoulder
Instability most commonly occurs due to separation of the ring of cartilage (the labrum), plus the capsule and shoulder ligaments attached to it, from the bone of the shoulder socket (referred to as a Bankart injury or tear):
Fig.2 Bankart Tear
Usually this is created by a complete dislocation of the shoulder. It may, however, result from an injury where the shoulder is stretched or wrenched in an abnormal direction but without actually dislocating.
A dislocation is most often towards the front (anterior) but in rarer circumstances may occur towards the back (posterior). In posterior dislocations the labral separation and ligament damage is at the back of
the socket.
An MRI is usually performed to outline the location and severity of cartilage (labral) damage in the unstable shoulder, often after the first dislocation.
Sometimes the capsule and ligaments alone become stretched without separation of the cartilage. This most commonly occurs in people who have loose ligaments around the body (‘double-jointed’).
Consequences of shoulder instability
The Bankart injury results in instability of the shoulder which can lead to:
Repeated dislocations of the shoulder – the younger the age at first dislocation, the greater the chance of experiencing another.
Feelings of looseness in the shoulder with the arm in certain positions or with certain activities
Lack of strength or confidence in the arm
Arthritis of the shoulder if present for many years
Treatment
Non-operative treatment of shoulder instability involves rest in a sling, physiotherapy and avoidance of the activities which lead to the feelings of looseness or which cause repeated dislocations.
The chance of a repeat dislocation or of having a shoulder which feels loose and doesn’t perform well with this type of treatment alone is very high in young active people.
Early surgical repair following a dislocation of the shoulder will result in less chance of dislocation later, as well as less looseness and more confidence in the arm. It is for this reason that surgical repair is now offered as a treatment option for a first dislocation in young people. The success of the surgery performed at this stage is higher than that following many months or years of shoulder instability and often numerous dislocations.
There is some evidence to show that the duration of instability and the number of dislocations relates to the long-term prognosis of the shoulder, particularly with respect to the development of arthritis.
In older or less active people, a non-operative approach to treating a first dislocation of the shoulder is preferred. Surgery can subsequently be performed if the shoulder continues to dislocate or subluxes frequently.
Bankart tear
Bankart tear – repair
Shoulder Stabilisation Surgery
Stabilisation surgery (shoulder “reconstruction”) is performed under general anaesthetic and usually via a keyhole (arthroscopic) technique.
2 or 3 small incisions ( 1 cm each) are made around the shoulder through which the camera (arthroscope) and plastic instrument tubes are inserted
Fig. 4 Shoulder Arthroscopy
The cartilage is repaired and the ligaments in front of the shoulder tightened with small stitches inserted through these holes. Pictures or video of the operation can be taken during the procedure. At the end the wounds are closed with an external stitch and then covered with a waterproof dressing.
The keyhole technique has some advantages compared with traditional methods of ëopení surgery using larger incisions:
Less pain
Shorter hospital stay (day case or overnight only)
Faster rehabilitation
Less stiffness (restriction of movement) following the surgery
Better ability to identify and treat other areas of damage
On rare occasions the procedure will need to be converted to one where a larger incision is made due to unexpected findings (such as a large fracture to the bone of the socket).
What to expect after shoulder surgery
You will wake up in the recovery area of the operating suite with a bulky dressing over the shoulder and a sling applied.
After surgery
Pain will be present however not extreme. By evening it should be well controlled with tablets. Occasionally a small dose of a strong pain killer given via injection is needed.
The shoulder will be swollen for approximately 24 hours due to collection of sterile fluid used during the operation to enable vision inside the joint.
Discharge from hospital is usual the following morning but may be in the same evening following a morning operation. The bulky dressing is taken down and the small waterproof dressings replaced if soiled. These should be left in place until the 2 week post-operative review by Mr. Dallalana, and the date of this will be given to you at the time the surgery is booked. You may shower but try not to directly soak the dressings each day.
A physiotherapist will see you prior to discharge and instruct you on simple exercises and management of the sling. The sling should be worn during the day when walking around, and taken off for brief periods when doing specific exercises and for showering. It does not need to be used at night, nor when seated.
You will receive a short (usually 5 day) supply of pain killing tablets to use at your discretion. This is usually a combination of paracetamol, an anti-inflammatory and an opiate such as endone or oxycontin. Reaction to the tablets may occur and can include a rash, nausea, stomach pain, dizziness and light-headedness. Stop them and see your local doctor for alternatives if needed.
The small wounds usually heal well with only a faint scar ultimately visible.
In the short term, the size of the muscle surrounding the shoulder will decrease due to lack of use. This will return following rehabilitation but will take many months.
Rehabilitation of the shoulder
The first 3 months after the surgery is critical for healing and to the overall success of the procedure.
The sling should be used for 6 weeks unless otherwise instructed.
After the first few days pain will settle down well – avoid the temptation to do too much too soon.
No elevation of the arm above shoulder height or excessive rotation outwards is permitted.
Most general duties of daily living should be performed with the other hand, however you may write and use a computer with the operated side, and use the arm to assist with eating.
Running should be avoided in this time.
Driving is not permitted while the sling is being used.
An exercise bike can be used almost straight away after surgery if desired
Phase 1 rehab – regain motion
It is normal to have a degree of stiffness in the shoulder following surgery and subsequent immobilization in a sling which needs to be overcome
Physiotherapy plus home exercises
From 6 weeks for stabilization surgery
Phase 2 rehab – regain strength
Physiotherapy plus gym program in some cases.
From 12 weeks post surgery
Phase 3 rehab – Return of muscle balance, co-ordination and full strength.
sport / activity specific physiotherapy plus ongoing strengthening work
Timing to full recovery and return to sport or work is variable and depends greatly on individual demands.
Running may resume at 6 weeks.
Swimming may resume at 4 months
Graded return to throwing or overhead sports should commence at 4 months, progressing to maximal loading by 6 months
Contact sport should be avoided for 5 to 6 months.
Non-physical work duties are appropriate from the time of removal of the sling, or before this as comfort allows in some situations. Return to heavy physical work with the involved arm will require 10 to 20 weeks depending on demands.
Possible complications after shoulder surgery
Complications are rare from this type of surgery.
Some complications which are related directly to the shoulder:
Bleeding under the skin related to the arthroscopy entry holes leading to local bruising. This bruising may run down the arm and across to the chest area. It is common, goes away in a couple of weeks, and does not require treatment.
Infection may occur and may be suspected by an increase in pain, fever, nausea and generally feeling unwell. The surgical wounds may be surrounded by reddening of the skin and may discharge fluid, blood or pus. There may be a foul odour. Infection around the small wounds only will settle without consequence after treatment to the area such as removing the stitch, local dressings and possibly antibiotic tablets. Infection deep within the shoulder is very rare however more serious when it occurs, and may require surgical washout of the shoulder along with prolonged courses of antibiotics. This type of infection may lead to permanent damage to the cartilage within the shoulder joint.
Stiffness (restricted movement) may occur despite appropriate rehabilitation with exercise and physiotherapy. It is uncommon. On occasions a brief procedure under anaesthetic may be required to free up the shoulder.
Failure of the procedure will result in re-dislocation of the shoulder, a return of a feeling of looseness, or persistent pain. This may happen due to the ligaments stretching out again or the cartilage (labrum) not adhering well to the bone. Failure usually occurs following another injury to the shoulder but may occur with only minimal trauma to the shoulder. Failure rates vary from 3% to 15% depending on individual circumstances, and this should be discussed specifically. Repeat surgery is often, but not always, required in the case of failure of the initial procedure.
Implanted material such as sutures and the plastic suture tacks in the bone can loosen and become prominent, rubbing on nearby cartilage or other structures.
Nerve injury resulting in weakness of the muscles around the shoulder or of the arm or hand, and / or loss of feeling in the skin in the same areas, have been reported following this type of surgery. It may result from stretching of the nerves during grasping and positioning of the arm during the surgery, or direct damage to the nerve from the arthroscope or arthroscopic instruments used. Nerve injury is usually temporary but rarely may be permanent. Permanent nerve injury may require grafting or other corrective surgery.
Injury the major blood vessels passing by the shoulder is possible however extremely rare. If this happens, surgery to reconstruct the artery or vein could be needed. Permanent loss of muscle function in the arm or hand may occur.
Some complications of a more general nature:
The surgery is carried out under general anaesthetic which is very safe, however on very rare instances a problem relating to the airway, lungs or heart and circulation may occur.
An intravenous line is always required, an often an additional line into a small artery near the wrist to monitor blood pressure. Its use may result in pain or bruising at the point of entry, and rarely an infection or thrombosis of the vein or artery.
Blood clots in the veins of the calf and / or leg (Deep Venous Thrombosis) may occur despite the surgery not involving these areas. It is very rare but when large can pose the threat of movement of the clots within the veins to the lungs (Pulmonary Embolus) and this can be serious or even fatal.
Your anaesthetist will discuss the use of an injection above the shoulder near the neck (Nerve Block) to help ëdeadení the shoulder and arm for approximately 24 hours to help control pain. There are complications reported relating to this including bruising and nerve damage. A nerve block is not often used with this particular type of keyhole surgery. You will be given contact details for the anaesthetist at the time of surgery booking.
Allergy to the antibiotic which is routinely used immediately prior to the surgery can occur. This most often causes a rash. Very rarely when serious an allergy can cause obstruction to the airway or reduced blood pressure.
In case of problems:
Pain control – contact local GP initially
Signs of infection (persistent increase in pain, wound discharge beyond 2 days following surgery, foul odour, fevers) – contact Mr. Dallalana via the rooms or through the hospital where you had your surgery if out of business hours. GP may be contacted for review concomitantly.
Tingling in the arm or hand or calf pain – contact Mr. Dallalana via the rooms or GP if convenient. Contact the hospital where you had your operation if out of hours.
numbness or persistent coolness in the hand or fingers – nearest emergency department
Shortness of breath, severe lack of energy or sudden high fevers with chills or shakes – nearest emergency department.
Non-urgent matters should be listed for discussion at the next review with Mr. Dallalana or alternatively queries can be directed via e-mail at dallar@parkclinic.com.au or by calling the rooms.
Certificates can be obtained at review or by your GP at other times.
Rooms at
71/166 Gipps St. East Melbourne 3002
and Suite 54, Cabrini Medical centre, Isabella St. Malvern
Phone (03) 8415 1907
(03) 9928 6555 (Mercy Private Hospital)
(03) 9508 1222 (Cabrini Hospital)
Email dallar@parkclinic.com.au