Mr. Richard Dallalana
MBBS FRACS FAOrthA
Background
Acromioclavicular or AC Joint Injury results from falling directly onto the point of the shoulder and is most commonly seen following a sporting accident. Mild injury results in pain at the top of the shoulder, short term restricted use of the arm, and does not require surgery. More severe separation can result in persistent symptoms which may include restricted function of the arm and will often require surgery.
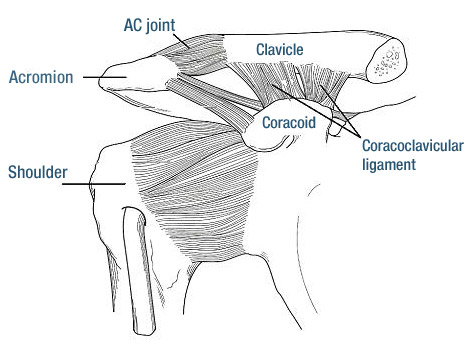
Anatomy (see fig. 1)
The area of interest lies just on top of the shoulder joint itself and involves the connection between the collar bone (clavicle) and a part of the shoulder blade called the acromion. The AC joint itself is a small joint which lies between the very outer tip of the collar bone and the acromion. It is made up of a small piece of cartilage sandwiched between the 2 bones and covered in a sack called the capsule. Relatively weak ligaments span between the 2 bones also. The collarbone is held firmly in place by these ligaments and also a set of much strong ligaments which run between the under surface of the collar bone and a projection of bone from the shoulder blade called the coracoid. These are called the coracoclavicular (C-C ligaments).
Fig. 1 AC joint area anatomy
Structural Damage and Consequences
In a mild injury there is a simple sprain of the ligaments and capsule of the AC joint (Grade I),or a partial tearing of the ligaments allowing slight separation of the AC joint (Grade II).
Fig.2 Grade I
Fig.3 Grade 2
These injuries result in pain and local swelling and in the case of Grade II injuries a permanent increase in the bump of the outer end of the collar bone. Grade I and Grade II injuries can be treated in a sling for a few weeks to allow pain to settle and thereafter by a physiotherapy program to ensure full movement of the shoulder is regained and to restore strength.
On rare occasions persistent pain from these injuries will require further treatment. An injection of cortisone in to the joint can help, and if not a small surgical procedure at a later stage. This will usually take the form of resection of the outer end of the collar bone and the associated capsule and ligaments of the AC joint.
A severe AC joint injury involves complete rupture of both the AC joint ligaments and the coracoclavicular ligaments. This results in a wide separation of the AC joint with elevation of the collar bone and subsequently a prominent bump and change in contour of the shoulder (Grade III).
Fig.4 Grade III
These ligaments do not heal by themselves and ongoing problems can occur. These may take the form of:
persistent pain in the area;
clicking or catching with movement of the shoulder in certain positions;
reduction of full strength in the arm;
restriction in the ability to carry out sporting activities particularly of a throwing nature, or work place duties where there is a requirement to frequently lift or manoeuvre objects at or above the shoulder height;
Treatment
Grade III AC separation can be treated with or without surgery and the decision regarding this needs to be individualised.
Non operative treatment for this injury is similar initially to that of Grade I or II injuries with the use of a sling until pain settles and thereafter physiotherapy to restore movement and strength. It may take 6-8 weeks for the pain to settle sufficiently to allow normal use of the arm and up to 3 months before adequate strength returns for competitive sport or overhead physical work. The prominent bump and change in shape of the shoulder will not change.
In some cases following this form of treatment adequate movement and strength with minimal or no pain will result in the ability to return to previous work or sporting activities. In other cases however significant persistent pain or feelings of clicking or catching or reduced strength will prevent return to previous activities.
Surgical treatment for this condition is undertaken when this situation arises. At this point the operation consists of a reconstruction of the coracoclavicular ligament with a graft of some kind (a nearby ligament, an artificial graft material, or both)
My recommendation is to consider having the surgery performed early after the injury (within the first few weeks) in people who engage in throwing or contact sports or those who perform overhead or heavy manual work.
In most others it is reasonable to take a non operative approach to this injury initially and undergo the surgery only if persistent symptoms become unacceptable. There is a higher chance that people with lower demands will not require the surgery.
Early Surgery: Acromioclavicular repair
In situations where the surgery is performed within the first few weeks of injury no graft is required to be used. The operation itself may be performed as a day case and consists of placement of an implant to hold the collar bone down to its normal location. This implant is either a metal plate (see picture) or a synthetic ligament substitute.
Fig. 5 Metal plate fixation
Later Surgery: Acromioclavicular Reconstruction Surgery
The surgery for a reconstruction of the AC joint involves a vertical incision of 3-4 cm over the front of the shoulder. The outer 1cm of the prominent collar bone is often cut off and the AC joint thus is replaced with scar tissue once healing has occurred. The strong coracoclavicular ligament which normally holds the collar bone down is reconstructed using either a hamstring graft harvested from the leg or using a small ligament which is nearby at the top of the shoulder. An implant is then added to provide initial strength to the area while the grafted ligament matures. The implant is either a metal plate or artificial ligament. The synthetic ligament is designed to remain in the body permanently but can be removed if necessary. The metal plate always requires removal at 3-4 months following the operation. A dissolving stitch is used at the end.
What to expect after the surgery
(the following comments apply to both the early repair and full reconstruction surgery.)
You will wake up in the recovery area of the operating suite with a bulky dressing over the shoulder and a sling applied.
Pain will be present but by evening should be well controlled with the tablets.
Discharge from hospital is usual the following morning but may be in the same evening following a morning operation. The bulky dressing is taken down and the small waterproof dressings replaced if soiled. You may shower but try not to directly soak the dressings. The wounds should be kept dry until the dressing is removed at 2 week review.
A physiotherapist will see you prior to discharge and instruct on simple exercises to do and how to manage the sling. In general the sling should be used when walking around for the first 4 weeks following surgery. It may be left off overnight. You may use the arm for eating, writing and typing and other similar light tasks.
You will receive a short (usually 5 day) supply of pain killing tablets to use at your discretion. Reaction to the tablets may occur and can include a rash, nausea, stomach pain, dizziness and light-headedness. Stop them and see your local doctor for alternatives if needed.
Rehabilitation
The goal of the early recovery period is to limit excessive force through the operated area. Any weight held in the hand or lifted with the arm has a tendency to separate the AC joint which is working against the goal of the surgery. Shoulder flexibility should be maintained during this time.
Once out of the sling, physiotherapy will be helpful to restore complete movement and regain strength
Sporting activity and manual labour may commence from the 3 month point if adequate strength has been regained.
Full recovery is usually 4 to 6 months.
Prognosis
In the majority of cases full use of the arm is expected.
Perfect positioning of the AC joint is not always achieved and some riding up of the collar bone may be seen down the track. This rarely requires repeat surgery and is mostly painless.
Occasionally persistent discomfort can occur and may require treatment.
A repeat procedure will be required if the metal plate is used to remove it at 3 to 4 months following surgery. This is a day case with little restriction to follow.
Possible complications
Complications are rare from this type of surgery.
Some complications which are related directly to the shoulder:
Bleeding under the skin related to the incision may lead to local bruising. This bruising may run down the arm and across to the chest area. It is common, goes away in a couple of weeks, and does not require treatment.
Infection may occur and may be suspected by an increase in pain, fever, nausea and generally feeling unwell. The surgical wounds may be surrounded by reddening of the skin and may discharge fluid, blood or pus. There may be a foul odour. Infection around the small wounds only will settle without consequence after treatment to the area such as removing the stitch, local dressings and possibly antibiotic tablets. Infection deep within the shoulder is very rare however more serious when it occurs, and may require surgical washout of the shoulder along with prolonged courses of antibiotics.
Stiffness of the shoulder joint itself due to the prolonged period in a sling may occur despite appropriate rehabilitation with exercise and physiotherapy. It is uncommon. On occasions a brief procedure under anaesthetic may be required to free up the shoulder.
Breakage of the metal plate, the bone near it or of the synthetic ligament graft has been reported.
It is common following this type of surgery to have a small numb patch over the top of the shoulder due to stretching or damage to a small nerve in the area of the incision. It does not always resolve with time and is of no particular consequence. Damage of important nerves which pass near the surgical area into the arm is possible however extremely rare.
Injury to major blood vessels passing to the shoulder is also possible. Some large vessels pass directly beneath the collar bone and are open to injury during surgery in this area. If this happens, surgery to reconstruct the artery or vein could be needed. Permanent loss of muscle function in the arm or hand may occur.
Some complications of a more general nature:
The surgery is carried out under general anaesthetic which is very safe, however on very rare instances a problem relating to the airway, lungs or heart and circulation may occur.
An intravenous line is always required, an often an additional line into a small artery near the wrist to monitor blood pressure. Its use may result in pain or bruising at the point of entry, and rarely an infection or thrombosis of the vein or artery.
Blood clots in the veins of the calf and / or leg (Deep Venous Thrombosis) may occur despite the surgery not involving these areas. It is very rare but when large can pose the threat of movement of the clots within the veins to the lungs (Pulmonary Embolus) and this can be serious or even fatal.
Your anaesthetist will discuss the use of an injection above the shoulder near the neck (Nerve Block) to help ‘deaden’ the shoulder and arm for approximately 24 hours to help control pain. There are complications reported relating to this including bruising and nerve damage. This nerve block is not commonly used for AC joint surgery.
Allergy to the antibiotic which is routinely used immediately prior to the surgery can occur. This most often causes a rash. Very rarely when serious an allergy can cause obstruction to the airway or reduced blood pressure.
In case of problems:
Pain control – contact local GP initially
Signs of infection (persistent increase in pain, wound discharge beyond 2 days following surgery, foul odour, fevers) – contact Mr. Dallalana via the rooms or through the hospital where you had your surgery if out of business hours. GP may be contacted for review concomitantly.
Tingling in the arm or hand or calf pain – contact Mr. Dallalana via the rooms or GP if convenient. Contact the hospital where you had your operation if out of hours.
numbness or persistent coolness in the hand or fingers – nearest emergency department
Shortness of breath, severe lack of energy or sudden high fevers with chills or shakes – nearest emergency department.
Non-urgent matters should be listed for discussion at the next review with Mr. Dallalana or alternatively queries can be directed via e-mail at dallar@parkclinic.com.au or by calling the rooms.
Certificates can be obtained at review or by your GP at other times.
Rooms at
71/166 Gipps St. East Melbourne 3002
and Suite 54, Cabrini Medical centre, Isabella St. Malvern
Phone (03) 8415 1907
(03) 9928 6555 (Mercy Private Hospital)
(03) 9508 1222 (Cabrini Hospital)
Email dallar@parkclinic.com.au